【SUMMARY】
Acute diarrhea disease in young children is a major cause of
morbidity worldwide and is a leading cause of mortality in developing
countries. Rotavirus is the most common agent responsible for acute
gastroenteritis, mainly in young children. Its discovery in 1973 and its
association with infantile gastroenteritis represented a very important
advancement in the study of gastroenteritis not caused by acute bacterial
infection. Rotavirus is transmitted by oral-fecal route with an incubation
period of 1-3 days. Although specimen collections taken within the second and
fifth day of the illness are ideal for antigen detection, the rotavirus may
still be found while diarrhea continues. Rotaviral gastroenteritis may result
in mortality for populations at risk such as infants, the elderly and
immunocompromised patients. In temperate climates, rotavirus infections occur
mainly in the winter months. Endemics as well as epidemics affecting some
thousand people have been reported. 4 With hospitalized children suffering from
acute enteric disease up to 50% of the analyzed specimen were positive for
rotavirus. 5 The viruses replicate in the cell nucleus and tend to be host
species specific producing a characteristic cytopathic effect (CPE). Because
rotavirus is extremely difficult to culture, it is unusual to use isolation of
the virus in diagnosing an infection.
Instead, a variety of techniques have been developed to detect rotavirus in
feces. Research has shown that enteric adenoviruses, primarily Ad40 and Ad41, are
a leading cause of diarrhea in many of these children, second only to the
rotaviruses. These viral pathogens have been isolated throughout the world, and
can cause diarrhea in children year round. Infections are most frequently seen
in children less than two years of age, but have been found in patients of all
ages. Further studies indicate that adenoviruses are associated with 4 - 15% of
all hospitalized cases of viral gastroenteritis. 5,6,7,8,9 Rapid and accurate
diagnosis of gastroenteritis due to adenovirus is helpful in establishing the
etiology of gastroenteritis and related patient management.
Other diagnostic techniques such as electron microscopy (EM) and nucleic acid
hybridization are expensive and labor-intensive. With the self-limiting nature
of adenovirus infection, such expensive and labor-intensive tests may not be
necessary.
The Rotavirus and Adenovirus Combo Test Cassette (Feces) is a rapid
chromatographic immunoassay for the qualitative detection of rotavirus and
adenovirus in human feces specimen, providing results in 10 minutes. The test
utilizes antibody specific for rotavirus and adenovirus to selectively detect
rotavirus and adenovirus from human feces specimens.
【DIRECTIONS
FOR USE】
Allow the test cassette, specimen, and buffer to reach room temperature
(15-30°C) prior to testing.
1. To collect fecal specimens:Collect sufficient quantity of feces (1-2 ml or
1-2 g) in a clean, dry specimen collection container to obtain enough virus
particles. Best results will be obtained if the assay is performed within 6
hours after collection. Specimen collected may be stored for 3 days at 2-8°C if
not tested within 6 hours. For long-term storage, specimens should be kept
below -20°C.
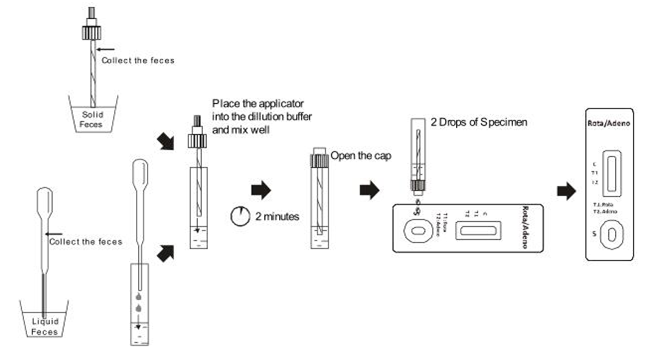
2. To process fecal specimens:
For Solid Specimens:
Unscrew the cap of the specimens,then randomly stab the specimen
collection applicator into the fecal specimen in at least 3 different sites to
collect approximately 50 mg of feces (equivalent to 1/4 of a pea). Do not scoop
the fecal specimen.
For Liquid Specimens:
Hold the dropper vertically, aspirate fecal specimens, and then transfer 2
drops of the liquid specimen (approximately 50 µL) into the specimen collection
tube containing the extraction buffer.
Tighten the cap onto the specimen collection tube, then shake the specimen
collection tubevigorously to mix the specimen and the extraction buffer. Leave
the collection tube for reaction for 2 minutes.
3. Bring the pouch to room temperature before opening it. Remove the test
cassette from the foil pouch and use it within one hour. Best results will be
obtained if the test is performed immediately after opening the foil pouch.
4. Hold the specimen collection tube upright and open the cap on the tip.
Invert the specimen collection tube and transfer 2 full drops of the extracted
specimen (approximately 80μL) to the specimen well (S) of the test cassette,
then start the timer. Avoid trapping air bubbles in the specimen well (S). See
illustration below.
5. Read the results at 10 minutes after dispensing the specimen. Do not read
results after 20 minutes.
Note: If the specimen does not migrate (presence of particles), centrifuge the
extracted specimen contained in the extraction buffer vial. Collect 80 µL of
supernatant, dispense into the specimen well (S). Start the timer and continue
from step 5 onwards in the above instructions for use.